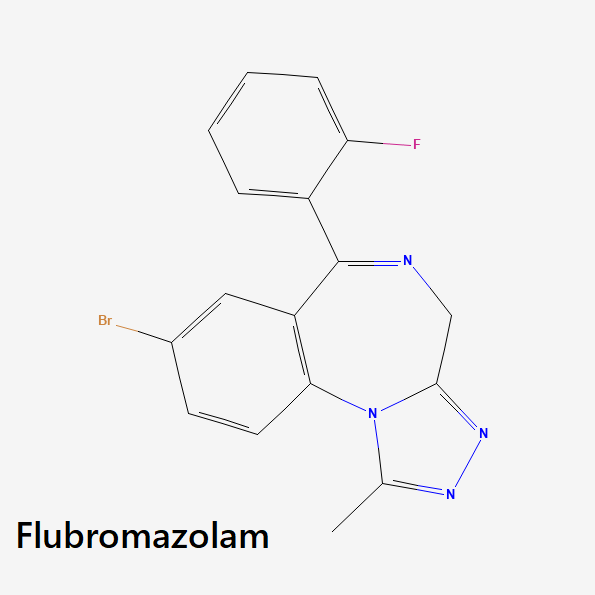
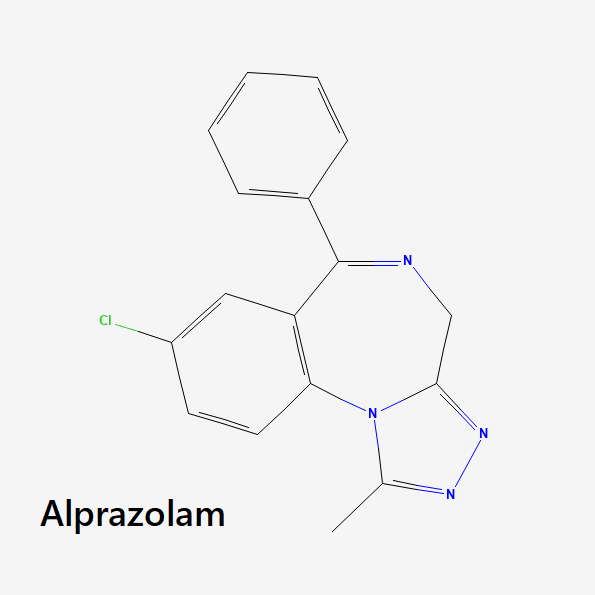
Flubromazolam, also known as “liquid Xanax” or JYI-73, is a triazolobenzodiazepine (TBZDs) analog of the designer benzodiazepine, flubromazepam.
The TBZD class of benzos is known for its elevated potencies and its strong emphasis on antidepressant properties.
Among all the dozens of benzodiazepines in existence, flubromazolam stands out by being the most powerful benzodiazepine in existence. This, of course, also makes flubromazolam an extremely dangerous compound.
Flubromazolam is so potent that a mere 0.2 mg dose is equivalent to a 10 mg dose of diazepam. It can be lethal in doses as low as 3 mg [1].
Flubromazolam does not have any accepted medical uses in the United States. Because of this, it is only available through unregulated online retailers and is primarily used as a recreational drug.
IUPAC Name
8-Bromo-6-(2-fluorophenyl)-1-methyl-4H-[1,2,4]triazolo[4,3-a][1,4]benzodiazepine
Other Names
Liquid Xanax, JYI-73
Metabolism
The metabolism of flubromazolam is hepatic and is at least partially mediated by the CYP3A4/5 and UGT1A4 enzymes [2], which implies that enzyme polymorphisms may influence the excretion and pharmacological effects of the compound.
Furthermore, flubromazolam’s primary metabolites are formed predominantly by hydroxylation, dihydroxylation, and O-glucuronidation, including α-hydroxy-flubromazolam (the most abundant metabolite), 4-hydroxy-flubromazolam, flubromazolam N-glucuronide, α-hydroxy-flubromazolam glucuronide, and 4-hydroxy-flubromazolam glucuronide.
Duration of Effects
Flubromazolam has an estimated terminal elimination half-life of 10–20 hours [2].
How Does Flubromazolam Work?
Flubromazolam exerts its pharmacological effects via the benzodiazepine receptor site located on GABA neurotransmitters in the brain and central nervous system (CNS). When benzodiazepines bind to these receptor sites, they increase the effects of GABA.
Simply stated, benzodiazepines slow down neuronal activity — causing sedation, disinhibition, muscle relaxation, and a release of anxiety.
The onset of action after ingestion is approximately 20 to 45 minutes. Self-assessment reports claim that the average duration of effects is three to six hours, while the after-effects may last from one to 14 hours [3].
In terms of effects, flubromazolam produces a wide range of benzodiazepine-related effects. It has anxiolytic, disinhibiting, sedative, muscle relaxant, and memory-suppressing actions. Part of flubromazolam’s exceptional potency is likely due to its extremely high affinity for GABA receptors.
Flubromazolam Pharmacokinetics
Research has shown that a single 0.5 mg flubromazolam dose induced strong sedative effects that lasted more than 10 hours and partial amnesia over more than 24 hours.
Studies have also identified an interesting particularity of flubromazolam. With the same 0.5 mg doses, researchers observed that flubromazolam has two peak serum concentrations. The first one was reached approximately 5 hours (7.4 ng/mL) after administration [2].
Is Flubromazolam Safe? Risks & Side Effects
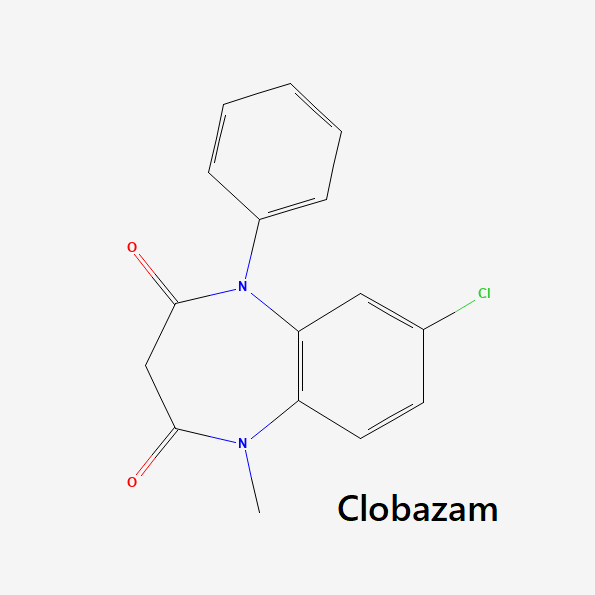
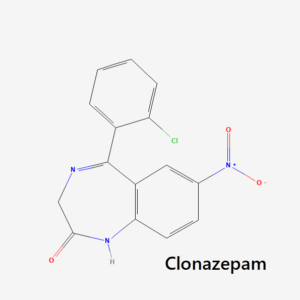
Most benzodiazepines are similar to each other in terms of their inherent levels of risk. There are still meaningful differences between them, mainly relating to factors such as potency, elimination half-life, how they interact with GABA receptors (partial or full agonists), etc. With that said, all benzodiazepines share the same Schedule IV classification under the Controlled Substances Act.
However, the situation is different when it comes to flubromazolam. The extreme potency of this compound means that the potential for severe health events is much more prevalent than with other benzodiazepines. As such, flubromazolam is not an approved medication in the United States or the wider world.
But people still manage to get their hands on flubromazolam and other restricted benzos. Medical authorities have detected flubromazolam use in countries like Australia, Denmark, Norway, Poland, Sweden, the USA, and Wales. Luckily though, from what data is available, it does not seem that flubromazolam is especially prevalent. For instance, the USA National Poisons Data System reported 13 cases of single-agent flubromazolam poisoning in 2016 and 2017. It is, therefore, less common in single-agent poisonings than etizolam, for example, which saw 106 cases over the same period [2].
Side Effects of Flubromazolam
Since flubromazolam is not an approved medication, there are not many clinical studies that attempt to evaluate its side effects profile. Most of the literature is based on reviewing forum posts on websites where recreational users go to describe their experiences with different types of drugs.
In these studies, it was found that flubromazolam was capable of causing a wide array of adverse effects, from mildly annoying to severely disabling. Among the most severe side effects reported were: severe substantial short-term memory loss, high degree of cognitive impairment, trouble while writing, talking, and walking, sleep paralysis, and other sleep-related affectations [4].
Furthermore, the DEA has warned potential users of flubromazolam of some of the effects of overdosing: severe intoxication associated with coma, hypotension, and rhabdomyolysis (a breakdown of muscle tissue leading to the release of dangerous protein into the bloodstream).
Alongside the severe affectations, users also commonly report the more traditional benzodiazepine-related side effects such as drowsiness, light-headedness, confusion, unsteadiness, dizziness, slurred speech, muscle weakness, memory problems, constipation, nausea, dry mouth, blurred vision [4].
The study mentioned above concluded that flubromazolam appears to be a highly addictive and precarious benzodiazepine with many, possibly severe, side effects. The substance is generally described as very potent and long-lasting. Memory loss and loss of control are common adverse effects, and withdrawals are severe for many users [4].
Benzodiazepine Withdrawal & Dependence
The ability of benzodiazepines to engender symptoms of physical dependence in users is a well-established fact. Almost all typical benzodiazepine share this trait, and it’s one of the major concerns doctors have to deal with when prescribing these medications.
However, there is a substantial difference between benzos when it comes to their dependence liability. Some benzos are known to be much milder than others in this regard. For example, partial agonist benzodiazepines like cinazepam and arfendazam are less adept at causing dependence than full receptor agonists.
Benzodiazepines with high dependence liability are usually those with higher potencies. This checks out in the case of flubromazolam, as self-assessment reports for flubromazolam consistently conclude that the drug presents a high dependence risk.
Studies that have examined these types of reports found that most users agreed on the rapid onset of tolerance effects of flubromazolam [4]. Some reported multiplying the dose after just a week’s use by even as much as 30 times the original dose to achieve the desired effects. However, this seemed more the case for those users whose main purpose was to get “high” and are, therefore, more likely to use high doses. “Self-medicating” users would typically retain the same low dosage over long periods to facilitate sleeping or handle anxiety.
If compared to other high-potency benzodiazepines, it is likely that flubromazolam can begin to create dependence symptoms in users in as little as seven to 10 days of consecutive use.
Reviews
There are no reviews yet.